Pressure Ulcer Prevention: Advice from the Experts
 March is National Bed Month, so we thought we’d share advice from the experts - our keynote speakers from the CLH Expo - about preventing and managing pressure ulcers and how the right bed can reduce the risk associated with pressure ulcers.
March is National Bed Month, so we thought we’d share advice from the experts - our keynote speakers from the CLH Expo - about preventing and managing pressure ulcers and how the right bed can reduce the risk associated with pressure ulcers.
At the #CLHExpo2018, we had the pleasure of hearing from two experts in pressure ulcer prevention, Annie Allsopp and Angela Harding, giving keynotes. The advice given was hugely beneficial and extremely useful, so we thought we’d share some of their top tips for preventing pressure ulcers, as well as managing them.
Something that both Annie and Angela focused on in their speeches was learning how to effectively spot the signs that there was the risk of a pressure ulcer and then taking steps to prevent the occurrence of one. It was also mentioned that there are certain facilities across the UK that have been pressure ulcer free for years, which shows that pressure ulcers are completely preventable if the right care and attention is provided.
An NHS led study found that pressure ulcers affect 20% of people living in nursing and care homes - that’s a huge percentage of older people across the UK. When you take this statistic into account and the fact that there are NHS trusts across the UK that have been pressure ulcer free for over five years, it’s clear that there is more that can be done to reduce the risk of pressure ulcers occurring.
Bearing that in mind, the question is what can be done to prevent pressure ulcers?
Risk assessment: For every patient or resident who enters a care facility or hospital, a risk assessment should be performed. There are various scales that can be used to determine risk, one of these is the Braden Scale. When it comes to preventing and treating pressure ulcers, risk assessments are crucial.
Skin inspections: On a regular basis, patient’s and resident’s skin should be checked for any signs of pressure-related damage. A tell-tale sign of an occurring pressure ulcer is red skin that doesn’t blanch when pressed, like a healthy area of red skin would do. Other signs of skin damage include skin that is hot to the touch, is swollen, and sore.
Take care of the skin: It’s vital that the skin is kept clean, dry and well hydrated. This can be particularly difficult in patients that are incontinent, as leaked urine can make pressure ulcers more likely to occur. Skin should be washed and dried regularly, and should always be kept clean and well hydrated. When drying skin, a patting motion rather than a rubbing motion is recommended, as this helps to keep the skin healthier and prevents the onset of pressure ulcers.
Incontinence: Often incontinence and pressure ulcers co-exist. This is because if incontinence isn’t properly managed, it can lead to the patient or resident being left with wet bedding or clothing, which can make pressure sores more likely to occur. That’s why utilising incontinence pads that offer the correct level of protection is vital, as is regularly checking for any leaks or wetness.
Nutrition: In addition to preventative skin care, good nutrition is vital for preventing pressure sores and aiding healing. It’s crucial that the diet of the patient or resident is regularly monitored and assessed, to ensure that they are getting all of the nutrients that they need. Adequate hydration is also crucial when it comes to preventing pressure sores.
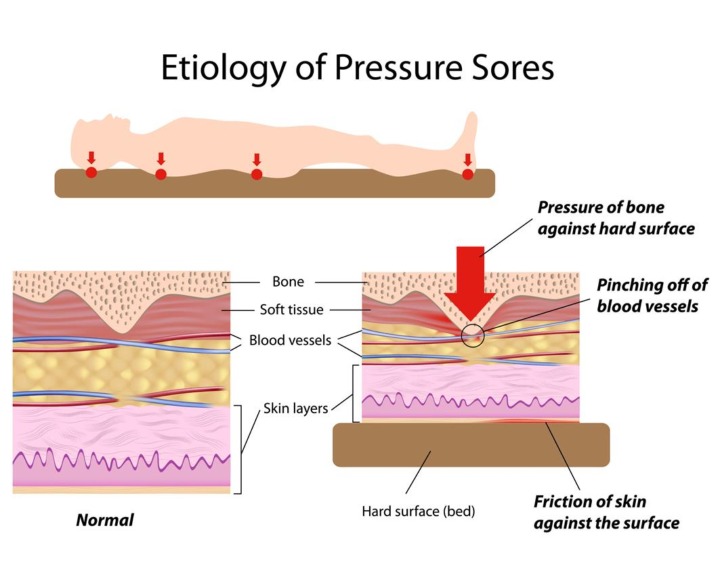
Position: When it comes to preventing pressure ulcers from occurring, the position in which a patient's body is placed is a vital factor. It’s important that all patients and residents are encouraged to regularly reposition themselves if they are able to do so. For any patients that aren’t able to naturally reposition themselves, it’s crucial that they are repositioned by your team on a regular basis - it used to be recommended that every two hours was how often repositioning is needed, but there is now some debate over whether this time frame is correct as it can differ depending on the pressure ulcer prevention products being used.
Pressure-redistributing equipment: For patients who are prone to pressure ulcers - once a patient gets one pressure ulcer, they are then more prone to developing them in the future - pressure re-distributing equipment can be highly effective. This includes mattresses that provide pressure reducing comfort that helps to reduce the risk of bed sores and increases patient comfort. There are various products to choose from for this, which is why consulting an expert in pressure care products is so vital, to ensure that you choose the right one for your needs.





